Long term damage is one of the biggest concerns after breaking a bone, or dislocating a joint. Bones typically heal in 6 weeks. However, post-traumatic arthritis can often develops 10 years later, even when the x-rays show a perfectly healed bone. This is a problem without a good solution. Over the past few decades there have been many advances in surgical treatments, however, the rate of arthritis following a trauma is mostly unchanged. Here are five things we know, and that promise answers in the future.
1) THE NUMBERS
About 12% of all arthritic joints that cause pain are due to post-traumatic changes, which is about 21 million cases, and an annual cost of $3 billion. A significant trauma to a joint will cause post-traumatic arthritis in about 75% of cases (that’s even when everything is done correctly).
2) CARTILAGE DAMAGE AT TIME OF INJURY
Cartilage is a great shock-absorber..when the shock is reasonable. But falling off a ladder for example, will impart a force to the ankle or knee joint that is beyond the capacity of cartilage to respond. Excessive force will irreparably destroy the cartilage and also squish the cells (chondrocytes) which heal and repair cartilage. Also the inflammation that occurs after the injury creates an bad environment for cartilage healing. After the injury the cartilage is simply gone. Surgeries to actually repair cartilage, or replace cartilage, are currently in preliminary stages of development (although there is a lot of future promise).
3) JOINT INSTABILITY
Cartilage isnt the only thing damaged during a traumatic injury. There are important ligaments that balance our joints to evenly distribute force across the cartilage. If these ligaments are torn, or even strained, the joint becomes less stable, and it cannot balance forces across it. Certain areas of the joint will experience significantly increased contract stress. This will lead to spots of accelerated cartilage wear and arthritis over time. Restoration of normal joint mechanics through surgery or bracing is critical for minimizing arthritis.
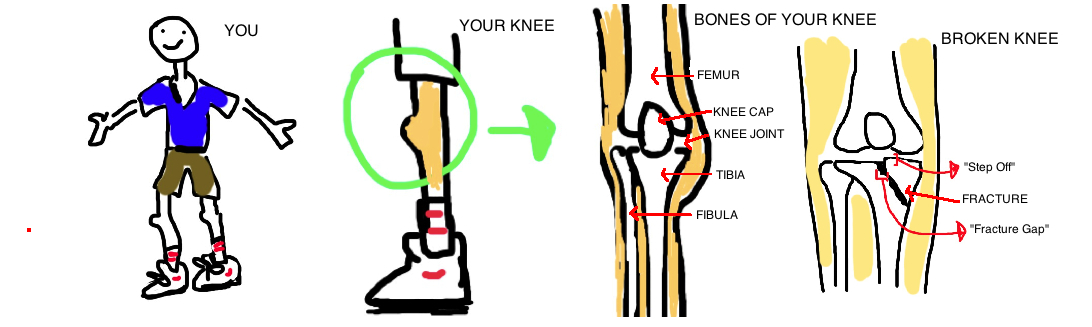
4) FRACTURE INTO A JOINT
A fracture line that enters a joint will creates an area of uneven cartilage (called a "step off") or a gap in the cartilage ("fracture gap"). A joint needs to move without friction to prevent arthritis over a lifetime of motion (a normal joint has less friction than ice on ice). Yet fractures into the joint create an uneven surface that increases friction, and speeds up cartilage wear. It causes certain areas of cartilage to bear more of the force across the joint, some studies stay over 300% of whats normal. Therefore surgery is almost always required when the fracture creates a joint line incongruity over 2 mm. Yet there is probably always some degree of micro-incongruity that occurs even after the fracture is repaired, and over time this may contribute to arthritis. Restoration of a normal joint line through surgery is critical for minimizing this risk for arthritis.
This is a common problem with ankle fractures (see talk) and knee fractures (see talk)
5) ARTHRITIS RISK DEPENDS ON WHAT JOINT WAS INJURED
Not all joints were created equally. The knee bears the weight of our entire body with every step. The wrist does not. Arthritis occurs as cartilage wears out with time, and cartilage wears out faster when it must bear more force. Knees are therefore at more risk than wrists for example (see talk: knee arthritis). Doctors treating fractures that enter the wrist joint often see signs of cartilage wear without patients complaining of post-trauamtic arthritis (see wrist fracture). However, in the knee, arthritic pain is predictably associated with post-traumatic changes to the joint, because the knee must balance more weight every day.