SPINE - BURST FRACTURE
our website is for educational purposes only. the information provided is not a substitution for seeing a medical doctor. for the treatment of a medical condition, see your doctor. we update the site frequently but medicine also changes frequently. thus the information on this site may not be current or accurate.
What is a Spine Burst Fracture?
A burst fracture is a very serious fracture of a vertebrae (the bones that make up our spine).
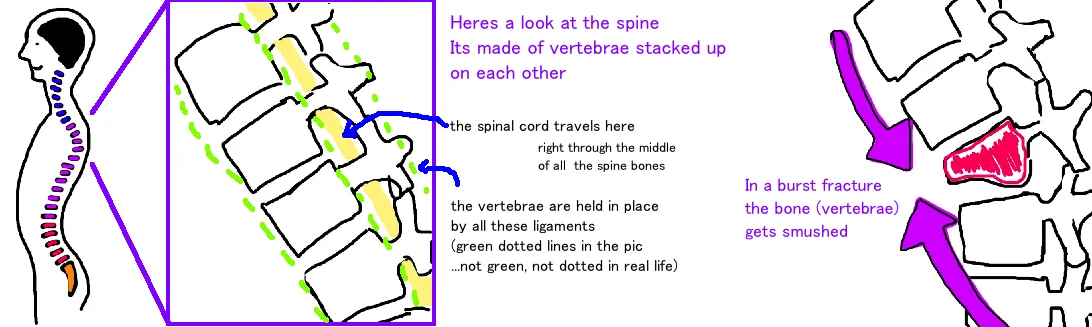
Lets quickly review some spine anatomy so we can better understand this injury.
There are seven vertebrae in the cervical spine (neck), 12 vertebrae in the thoracic spine (mid back), and 5 vertebrae in the lumbar spine (lower back). The vertebrae are stacked on each other like blocks. This forms the spine. The spine gives structural support that holds the body upright, and it protects the spinal cord. The spinal cord travels through the center of each vertebrae. There are many strong ligaments which hold the vertebral bodies in position to prevent any displacement which could damage the spinal cord.
The vertebrae are bones, and they can break like any other bone if they sustain a great enough force.
Overall the spine can be divided into three columns (a front, middle, and back) which contribute support to the stability of the spine.
A Burst fracture occurs when there is a significant compressive force on the front and middle column that not only squishes the bone, but also pushes some of the bone backward, into the spinal canal (which can be very dangerous as it often puts pressure on the spinal cord). The spinal canal is a narrow space within the vertebrae (theres no wiggle room here), so even a small piece of bone can press on the spinal cord and cause neurologic injury.
If the front and middle column of the spine break, it is called a “Two Column Injury”, if all three columns break then its called a "Three Column Injury". The majority of Burst fractures occur at the transition zone from the Thoracic Spine to the Lumbar Spine (called the Thoracolumbar Junction). The vertebrae most commonly affected (the ones getting squished) are L1, T12 and L2 (in that order).
How is a Spine Burst Fracture diagnosed?
A Burst Fracture occurs after a high-energy injury, most commonly a car accident. Its suspected when a person complains of severe back pain, with or without neurologic symptoms (like numbness or weakness below the painful area of the spine).
X-rays are often the first step in evaluating a spine fracture, however, in may Emergency Rooms these days, patients that come in after sustaining high energy injuries are wisked away to the CT scan before getting x-rays. CT scans are like many x-ray slices taken from multiple angles, which give a 3D picture of the spine and are very helpful in evaluating the spinal fracture and identifying all of the smaller bone fragments.
An MRI is often ordered as well to look at swelling in the spinal cord itself (a CT scan is great at showing bone, but not very helpful in showing nerve injury). In addition to getting all of these images of the spine, a very detailed neurologic examination is necessary to determine the degree of spinal cord damage, and also to localize the site of injury. By assessing where a patient is feeling muscle weakness or numbness, doctors are able to pinpoint which vertebrae in the spine are likely to be damaged.
How is a Spine Burst Fracture treated?
The goals of treatment is the restoration of a pain-free state, the preservation of a mobile/functional spine, and the prevention/reduction of neurologic injury.
The treatment approach for a Burst Fracture first focuses on the degree of neurologic symptoms.
If a patient has signs of spinal cord injury, and the CT scan or MRI shows a high likelihood of injury to the spinal cord, then surgery is recommended. The surgery is performed to take pressure off the spinal cord, and to stabilize the broken vertebrae with metal rods and screws to prevent the injury from become worse as the bone fragment can shift further out of position.
Treatment of a Burst fracture without signs of neurologic injury is more controversial.
The primary goal is to protect the spinal cord, and prevent the injury from getting worse. This is done by determining the amount of spine instability (a stable spine has a low chance of getting worse, while an unstable spine has a high chance of getting worse and causing new neurologic injury). If the vertebrae are significantly crushed (50% shorter than normal) or if they are significantly bent (over 30 degrees) or of the ligaments in the back of the spine (the posterior longitudinal ligament) is torn, then surgery is likely helpful in preventing further spine collapse (called a kyphosis deformity: where the spine bends too much at the site of injury).
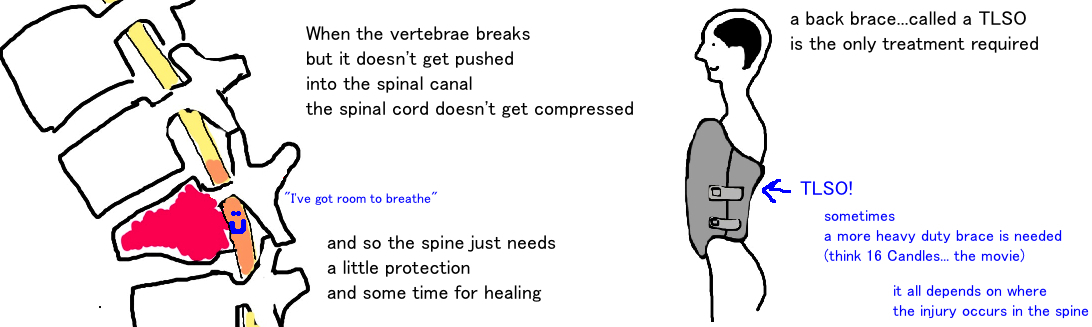
However, if there is a fracture but the spine is not significantly deformed, then patients can be treated safely with a brace that goes around the chest and back to provide stability while the injury heals.
What is the long term outcome?
Stabilizing the spine is the key to ensuring progressive healing. A brace is often successful at allowing the spine to heal without risk for future neruologic injury, although an abnormal curve in the back ("kyphotic deformity") following the injury is often greater than the same injury treated with surgery.
Surgery is a valuable treatment option in many situations that gives good long-term outcomes. Surgery to correct a kyphosis deformity is effective, although with time, some of the correction is lost (some degree of kyphosis develops around the site of injury), although this doesnt appear to cause new symptoms.
Unfortunately, spinal cord injury may or may not recover, this is an area that medicine is still in the learning stages. Younger people typically have a better chance at recovery, less severe injuries recover better, and earlier intervention also may lead to better recovery (however, the timing of intervention is also an area of controversy).
Reference
1) Denis F. Spinal instability as defined by the three-column spine concept in acute spinal trauma. CORR 1984; 189: 65-76. full article. classic review of spine trauma.
2) Gnanenthiran SR, Adie S, Harris IA. Nonoperative versus operative treatment for thoracolumbar burst fractures without neurologic deficit: a meta-analysis. CORR 2012; 470: 567-77. full article.
3) Chou PS et al. Fusion may not be a necessary procedure for surgically treated burst fractures of the thoracolumbar and lumbar spines. JBJS 2014; 96: 1724-31. full article.
4) Daniaux H et al. Application of posterior plating and modifications in thoracolumbar spine injuries. Indication, techniques, and results Spine 1991; 16: 125-33. full article. surgical approach to burst fx.
5) Wood K et al. Operative compared with nonoperative treatment of a thoracolumbar burst fracture without neurological deficit: A prospective, randomized study. JBJS 2003; 85: 773-781. full article. surgery isnt better in neuro intact pt.