BUNION
(Hallux Valgus & Hallux Rigidus)
our website is for educational purposes only. the information provided is not a substitution for seeing a medical doctor. for the treatment of a medical condition, see your doctor. we update the site frequently but medicine also changes frequently. thus the information on this site may not be current or accurate.
related talks: small toe deformity; broken foot (jones fracture); broken foot (lisfranc fracture);
What is a Foot Bunion?
A bunion is a boney prominence at the base of your big toe due to 1) arthritic changes or 2) malalignment of the bones at the joint (metatarsophalangeal joint).
There are two separate conditions that can cause a bunion.
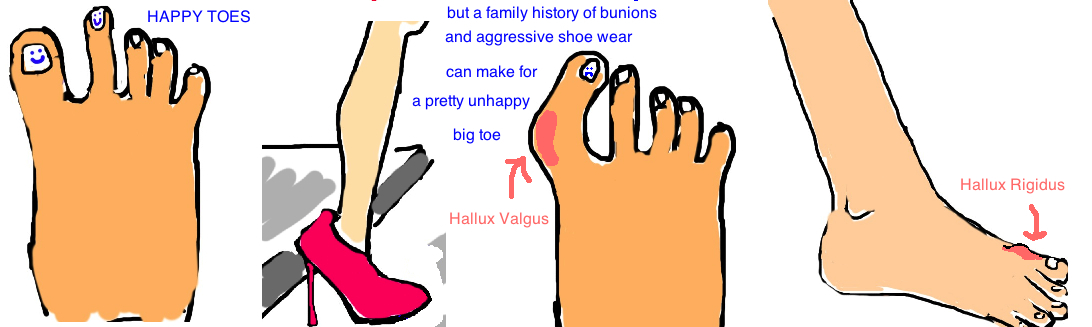
1) Hallux valgus (the most common) is a bunion that forms on the side of the big toe.
2) Hallux rigidus is a bunion that forms over the top of the big toe.
Lets talk about each separately.
1) Hallux valgus is much more common in women (some studies say almost 15:1 female to male ratio for this condition). This condition has been linked to high heels (referred to as shoes with a "narrow to box") and to genetics predisposition (about 70% of people who develop this condition reporting a family history). Other risk factors for developing this condition is ligament laxity, rheumatoid arthritis and flat feet. So the questions is what keep a normal big toe straight, and what goes wrong for it to curve? There is an important muscle that runs along the bottom of the foot (called the flexor hallicus brevis, "FHB") that attaches to both sides of the big toe and helps you flex this toe. But equally importantly, it also acts like reins on a horse where both sides are under equal tension so the big toe is directed straight. But, if long term pressure pushes on the big toe (like wearing high heels) then the "reins" of the flexor tendon will end up on just one side and thus pull the toe in one direction (instead of keeping it straight). Other factors contribute as well. The big toe joint capsule will become loose for constant pressure and will allow the bones to shift, and remember, if a person genetically has looser ligaments and tendons, the whole process will occur faster. Over time a bunion will develop on the inside of the foot.
2)Hallux Rigidus is arthritis of the big toe joint (called the 1st MTP joint). Even though arthritis is uncommon overall in the foot and ankle, the big toe is a common location when it does occur. Erosion of the big toe’s joint causes an irregular joint profile and a spike of bone forms at the top of your foot, called an “osteophyte”. This irregularity causes limited motion and pain (especially when the big toe moves upward)
How is a Foot Bunion diagnosed?
Most people can look at their foot and see the bunion that’s causing them pain and discomfort. A bunion is a structural problem with the big toe, so most people come to the doctor saying “My foot doesn’t fit comfortably into normal shoes, I have pain over this large bump that didn’t used to be there.” In hallux valgus the bump is along the inner portion of the foot, while the bump in hallux rigidus is along the top. Patients with hallux rigidus also complain of sharp pain when they take their first step in the morning (pushing off their big toe really hurts).
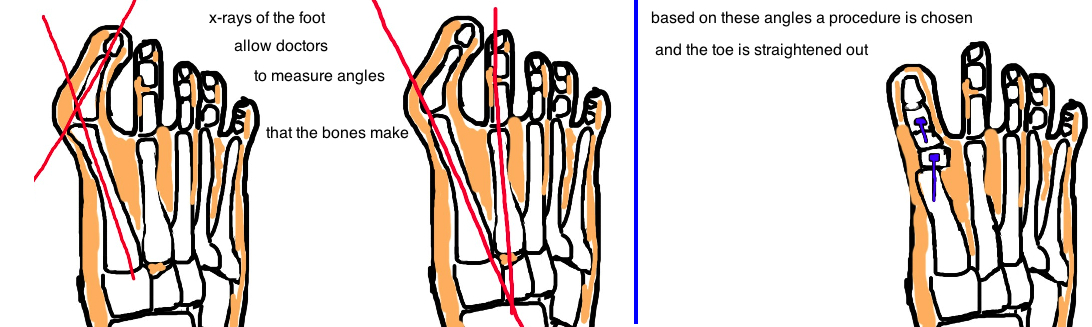
Diagnosis also made with x-rays. In hallux valgus, a measure of the alignment of the big toe bones (there are three bones that should be straight but become curved) is used to evaluate the severity. Hallux rigidus x-rays will show arthritic joint changes.
How is a Foot Bunion treated?
The two conditions are actually treated very differently. Even though they are both “bunions” they are caused by different things, and therefore require different approaches for treatment.
Hallux Rigidus (a bump on the top of the big toe) treatment depends on severity. If its caught early on, nonoperative treatment is recommended initially, and this includes special orthotics and stiff-soled shoes. If the condition is more advanced, then a procedure called a “Cheilectomy” is performed whereby the joint irregularity is smoothed out and the osteophyte (that spike of bone that forms) is removed. If the condition is much more advanced, and there is significant degeneration of the joint cartilage, then the joint is fused, thereby preventing any motion within the joint. This makes the joint stiff, but it also prevents pain, because pain occurs with movement in a joint without cartilage (cartilage reduces friction and allows bones to glide smoothly against each other at a joint).
Hallux Valgus (bump on the inside of the big toe) treatment also depends on severity.
In all medical fields there is currently a big push toward prevention. And it makes sense: the earlier you catch a problem, the easier it is to treat. It is much simpler to prevent a toe from bending, than it is to straighten a bent toe. With that in mind, if a patient comes in with a very small bunion, many doctors will initially recommend that the person change shoes. That alone may prevent the bunion from getting worse and may even make it better. However, once the toe is significantly bent, surgery is recommended if pain is persistent. You never "need" surgery for a painful toe, its not life threatening, rather, its recommended if it presents as a bother. Some surgeons will realign the bones by re-balancing the soft tissue (called a modified McBride procedure), meaning they will loosen and tighten certain areas of the joint capsule and surrounding ligaments. However, with current knowledge and experience, surgeons almost never perform this procedure alone because there is a high chance the bunion will recur. Instead, most surgeons recommend performing this soft tissue re-balancing in addition to reshaping one of the bones orrealigning one of the joints. In mild or moderate cases the metatarsal bone will be reshaped (a Chevron osteotomy), while in more severe cases the tarsometatarsal joint will be fused in a better aligned position (called a Lapidus procedure).
What is the long term outcome?
Most cases of hallux valgus or hallux rigidus are successfully treated with full resolution of symptoms. There are risks however to all procedures. One of which is a condition called hallux varus, which occurs when a doctor is overly aggressive in their surgical treatment of hallux varus. The big toe will look as if its running away from the others. The correction for this procedure can be soft tissue rebalancing, or creating a “artificial” ligament using fibrowire to realign the toe. The third option is the fuse the toe in the correct position. There is a high rate of successful correction for this deformity.
References
1) Torkki M et al. Surgery vs orthosis vs watchful waiting for hallux valgus: a randomized controlled trial. JAMA 2001; 16: 2474-80. full article. treatment outcomes.
2) Ferrari J et al. Interventions for treating hallux valgus and bunions. Cochrane Database Systematic Review. 2004. full article. no difference in surgical techniques.
3) Trnka HJ et al. Six first metatarsal shaft osteotomies: mechanical and immobilization comparisons. CORR 2000; 12: 256-65. full article. surgical technique comparisons.
4) Park HW et al. Comparison of outcomes between proximal and distal chevron osteotomy both with supplementary lateral soft-tissue release, for severe hallux valgus deformity: A prospective randomised controlled trial. JBJS 2013; 95: 510-6. full article. surgical technique comparisons.
5) Trnka HJ et al. The chevron osteotomy for correction of hallux valgus. Comparison of findings after two and five years of follow-up. JBJS 2000; 10:1373-8. full article. chevron is effective treatment for mild mod deformity.
5) Easley ME, Trnka HJ. Current concepts review: hallux valgus part 1: pathomechanics, clinical assessment, and nonoperative management. Foot Ankle Int 2007; 28: 654-9. full article. review.
6) Easley ME, Trnka HJ. Current concepts review: hallux valgus part II: operative treatment. Foot Ankle Int 2007; 28: 748-58. full article. review.
7) Coughlin MJ, Shurnas PS. Hallux Rigidus. Grading and long-term results of operative treatment. JBJS 2003; 85: 2072-88. full article. chielectomy is good for grade 1, 2, and fusion good for grade 3,4.
8) Shereff MJ, Baumhauer JF. Hallux rigidus and osteoarthrosis of the first metatarsophalangeal joint. JBJS 1998; 80:898-908. full article. review.
9) Sammarco VJ, Nichols R. Orthotic management for disorders of the hallux. FOot Ankle Clin 2005; 10: 191-209. full article. efficacy of nonop.
10) Gibson NJ, Thomson CE. Arthrodesis or total replacement arthroplasty for hallux rigidus: a randomized controlled trial. Foot Ankle Int 2005; 26: 680-90. full article. arthrodesis superior.
11) Brage ME, Ball ST. Surgical options for salvage of end-stage hallux rigidus. Foot Ankle Clin. 2002; 7: 49-73. full article. keller vs arthrodesis.