BROKEN KNEECAP
(PATELLA FRACTURE)
our website is for educational purposes only. the information provided is not a substitution for seeing a medical doctor. for the treatment of a medical condition, see your doctor. we update the site frequently but medicine also changes frequently.
related talks: kneecap dislocation; broken knee, runners knee
What is a Broken Kneecap (Patella Fracture) Fracture?
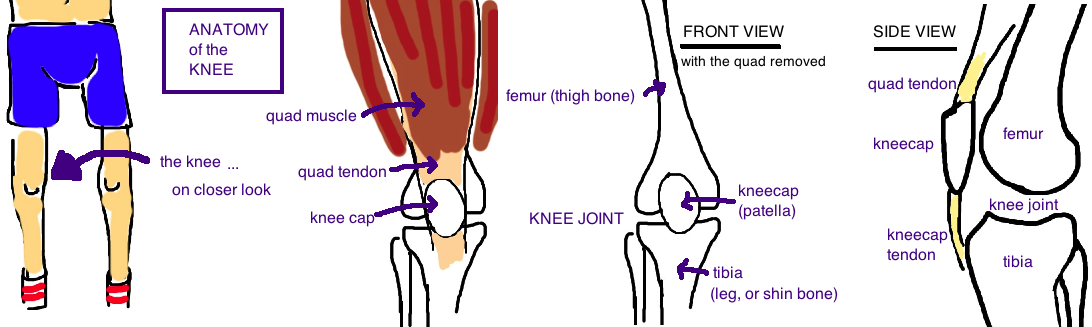
The kneecap is actually a bone located within the quad tendon and it helps you straighten your leg (technically speaking, it gives the quad muscle mechanical leverage for extending the leg).
The kneecap is a small bone and it can break if whacked too hard. It can also break if your knee is rapidly flexed causing the tendon to pull off the bone (called an “avulsion” fracture).
How is a Broken Kneecap (Patella Fracture) diagnosed?
People with a broken knee cap complain of significant pain and swelling around the knee.
They describe a direct trauma to the knee (whack!) or hyper-flexing their knee and then feeling significant pain. A kneecap fracture will usually prevent the quad tendon from working properly, so people with this injury cannot straighten their leg. This is an important diagnostic test to determine the severity of the injury. X-rays are the best test to confirm a kneecap fracture. A side view of the knee will show a break in the bone, and usually the force of the quad muscle will pull the fragment apart. The larger fragment of the kneecap will usually end up a few centimeters higher than normal.
How is a Broken Kneecap (Patella Fracture) treated?
The kneecap is important for daily function so its important that the fracture heals in a correct position.
If the break is minor like a hairline crack...meaning theres less than 2 mm of space between bone fragment then surgery can be avoided.
If the quad muscle can still fully straighten your leg then surgery can also be avoided.
If the decision is "no surgery", then the leg is braced with the knee completely straight for 2 weeks, and then range of motion is slowly started to prevent stiffness.
In most cases our strong quad muscle pulls the bone fragments apart, overlengthening the extensor mechanism (the quad tendon + kneecap + patellar tendon + retinaculum which work together to straighten our knee). As a result we cannot straighten our knee and we cannot rely on our body to heal itself in the correct position. Surgery is needed to put the bone fragments back together, and hold the pieces together with a metal wire (called a “tension band technique with cerclage wire”). It looks like the knee cap is tied together in a little bow.
In cases of an “avulsion” injury, where a small chip of bone is pulled off with the quad tendon, the goal of surgery is to reattach the tendon to otherwise intact kneecap (the small chip of bone is just removed).
On rare occasions, the injury is so bad that the kneecap is in too many pieces to fix (its turned to dust). In such cases the every effort is made to save as much of the kneecap as possible (there are no major problems if 25% or less of the bone is removed), however, if necessary, the entire bone can removed, which weakening the quad force by 50%.
What is the long term outcome?
Overall the kneecap heals well, and patients return to their normal activities after treatment.
Nonsurgical treatment of nondisplaced fractures has 98% good or excellent results. However, nonsurgical treatment of displaced fractures leads to 50% of people having notable limitations in daily activities.
Surgical treatment typically restores full function to the injured knee, and minimizes future pain, with good to excellent results in about 85% of people. Dissatisfaction with treatment usually occurs because theres very little soft tissue around the kneecap (that’s why its so easy to feel) and so the wire used in surgery can irritate the skin. About 20% of patients will choose to undergo a second surgery to remove the wire once the bone heals (the wire holds the bone fragments together during healing, so once the bone heals, the wire has no function). The kneecap is also a thin piece of bone, particular in the elder who have osteoporosis, so it can be difficult to obtain a sturdy repair of the bone. About 20% of fractures will show some signs of fragment separation during the healing process (this is not always painful, but it shows that healing can be a challenge). Post-traumatic arthritis is long-term complication of kneecap fractures.
The kneecap has the thickest cartilage of any bone in the body, and this indicates how much stress the bone must tolerate as it moves within the knee. Any injury powerful enough to break the bone, will probably also cause an injury to the cartilage, yet cartilage injury isn’t a initial focus because it doesn’t show up on x-ray (but it can be seen on MRI). The ultimate effects of the cartilage damage are often not appreciated until years later when the cartilage wears out faster than expected and people experience arthritic pain.
Reference
1) Melvin JS, Mehta S. Patellar fractures in adults. JAAOS 2011; 19: 198-207. full article. review.
2) Cameron JC. Transverse fracture of the patella. Glasgow Med J 1878; 10: 289-94. first orif patella in scotland with wire (soon repeated by Lister and Trendelenberg).
3) Watson-Jones R. Excision of the patella. Br J Surg 1945; 2: 195-6. interesting historical prospective. acclaimed surgoen watson-jones believed patella inhibited quad fxn, and patellectomy improved knee strength.
4) Albanese SA et al. Knee extensor mechanics after subtotal excision of the patella. CORR 1992; 285: 217-222. full article. in comminuted fx, need to salvage >75% patella to maintain near normal biomechanics. patella displaces tendon away from center of knee rotation, increasing moment arm (better mech advantage by 50%)
5) Lieb F, Perry J. Quadriceps funciton. JBJS 1968; 50: 1535-48. full article. double torque req. for terminal 15 degees of extension vs requirement for full flex to 15 degrees extension.
Treatment
1) Bostrom A. Fracture of the patella. A study of 422 patellar fractures. Acta Ortho Scand 1972; 143: 1-80. full article. 98% excellent result at 2 years. newer studies recommend early weight bear in extension.
2) Pritchett JW. Nonoperative treatment of widely displaced patella fractures. Am J Knee Surg 1997; 10: 145-7. full article. nonop due to comorbidity, 9/18 pt had notable limits in daily activity.
3) Burvant J et al. Evaluation of methods of internal fixation of transverse patella fractures: a biomechanical study; JOT 1994; 8: 147-53. full article. compared tension band, modified tension band over k-wire, screws, screws and tension band: using k-wire with cerclage is strong. but screws with cerclage is best
4) Chen A et al. Comparison of biodegradable and metallic tension-band fixation for patella fractures. Acta Orthop Scand 1998; 69: 39-42. full article. clinical outcome 2 yrs shows ethibond just as good as cerclage but less skin irritation.
5) Gosal HS et al. Clinical experience of patellar fracture fixation using metal wire or non-absorbable polyester: A study of 37 cases. Injury 2001; 32: 129-35. full article. ethibond is superior for patient satisfaction, equal union rates.
6) Böstman O et al. Comminuted displaced fractures of the patella. Injury 1981;13:196-202. full article. good outcome partial patellectomy for comminuted fx, unless >40% removed.