BROKEN HIP
aka...
(FEMORAL NECK FRACTURE)
(INTERTROCHANTERIC FRACTURE)
(SUBTROCHANTERIC FRACTURE)
our website is for educational purposes only. the information provided is not a substitution for seeing a medical doctor. for the treatment of a medical condition, see your doctor. we update the site frequently but medicine also changes frequently.
What is a Broken Hip (Hip Fracture)?
A broken hip is unfortunately one of the most common orthopedic injuries in the aging population.
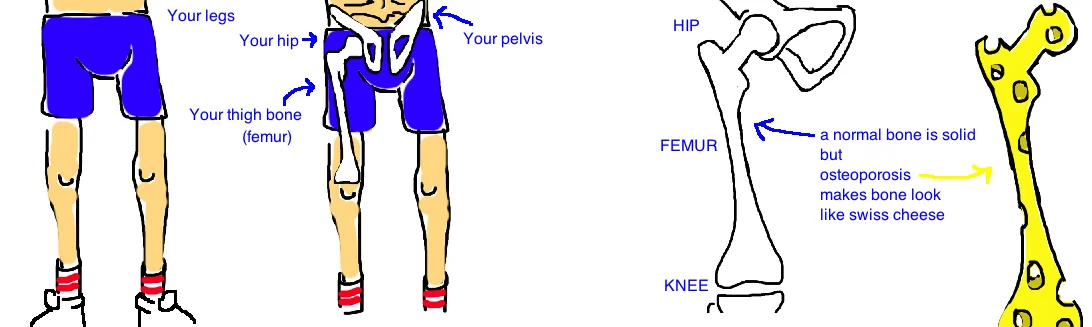
These fractures typically occur after a slip and fall. In a healthy young adult it would be very unusual for this type of fall to cause a broken hip, however, as we get older our bones naturally become osteoporotic (bones become thin.. its like the bone start to look like swiss cheese), and this makes our bones more prone to breaking.
The vast majority of broken hips occur in the elderly, however, a young person can also break a hip but it usually requires a major accident, like a high speed car crash.
To better understand this injury, lets quickly review the anatomy of our hip.
The hip joint is a “ball-and-socket” joint where your thigh bone (the femur) joins with the pelvis (the acetabulum). The femur is the “ball” while the pelvis is the “socket”, and hip fractures are an injury to the “ball” portion of the joint. The femoral neck is part of the femur just before it forms the hip joint, and its commonly broken because it is a narrow portion of bone. The connection between the femoral neck and femoral shaft contains two bony prominences (where muscles attach) called the “greater and lesser trochanter”. This is also a part of the femur that experiences a lot of stress during a fall and is commonly broken. The third location, the subtrochanteric fracture, occurs just below the “lesser trochanter” and this fracture pattern is usually seen in people that are taking bisphosphonate medication (used to treat osteoporosis).
There are 3 types of broken hips:
1) A fracture at the femoral neck; 2) a fracture at the trochanters (intertrochanteric); and 3) a fracture below the trochanters (subtrochanteric). Each of these fractures occur at a different location in the hip... and each is treated differently.
How is a Broken Hip (Hip Fracture) diagnosed?
Someone with a broken hip will report falling down, often just from standing height, which doesn’t sound impressive, but with osteoporosis, our bones are brittle and that’s all it takes. After the fall, people are unable to put weight on the injured leg and they report pain in the hip that radiates to their groin.
X-rays of the hip and pelvis will diagnose the break. Also, the fracture pattern seen on x-ray will allow the surgeon to offer the best treatment.
Sometimes people will come in with a story of falling, and will have all of the symptoms of a hip fracture, but the x-rays won't show anything.
In this case, a CT scan or MRI is ordered to look for a very small (“hairline”) fracture that may not show up on x-ray.
How is a Broken Hip (Hip Fracture) treated?
The best treatment for all types of hip fracture is determined by our body’s ability to heal the broken bone.
Our bones need nutrients to heal.
Our bones are not like rocks (a hard, unchanging mineral) but rather are living things that house millions of bone cells (called osteocytes) that rebuild the bone after a break. These cells normally get their nutrients from the blood (think of a flower needing water). However, with some hip fractures, the blood supply is injured, and the cells lose their ability to rebuild and the bone will wither and die like a plant that doesnt get watered. In the case of a hip fracture, the bone never heals (called a nonunion) and sometimes the “ball” portion of the hip crumples up (called avascular necrosis: "AVN").
The Femoral Neck Fracture has the highest risk of injury to the blood supply. This risk is influenced by certain things, like a person’s age, if they smoke, how far the bone fragments moved apart during the injury and how quickly a surgeons fixes the fracture (this last point is very controversial).
In cases where the bone fragments move apart, 80% will develop a disruption in the blood supply if not treated with surgery (surgery reduces the risk to 15-25%). In people under 60 years old, the bone fragments move apart 85% of the time, and in people over 60, they move apart 97% of the time.
Even in cases where the bone doesn’t move apart during the initial injury, there is still a 33% chance they will move within the next few weeks if surgery isn’t performed.
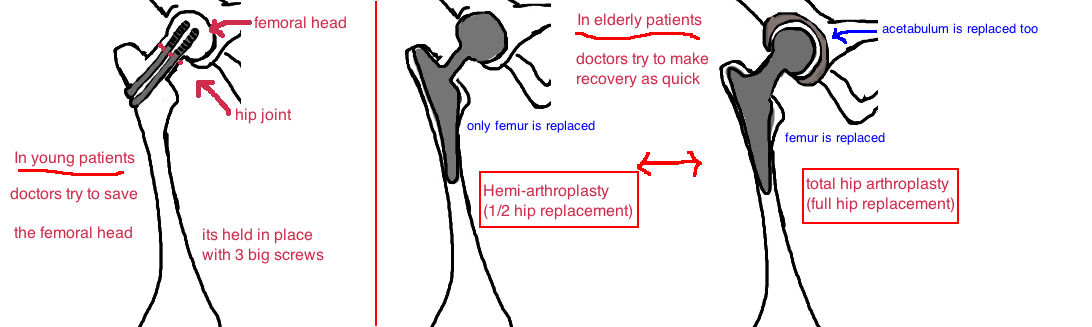
In younger people (less than 60 years old) we do everything we can to protect the blood vessels that supply the fractured bone. Surgery is performed urgently to realign the bone fragments (this straightens out any blood vessel that is kinked) and three screws are inserted to hold the bone in place while it heals. Surgery performed within 24 hours of the injury has better outcomes. There is still the risk that the bone doesn’t heal and the patient will need a second surgery to treat the unhealed or dead bone (about 10-25% risk). But in young people, the chance to save the natural hip joint is worth the risk of a revision surgery. This is not true in elderly patients (over 60 years old), where the goal of treatment is to maximize their recovery and rehabilitation from the injury.
In the elderly, a hip fracture can be a life threatening condition, not in the sense that they lose too much blood, but in terms of the injury being such a shock to the body that recovery (getting out of bed and back to a normal routine) becomes an insurmountable hurdle. Therefore most surgeons believe the setback from a non-healed fracture is too great a risk. Instead of trying to save the bone surgeons will immediately replace the broken bone (the “ball”) with a metal replica. This is half of a hip replacement (called a “hemi”). If the “ball” and “socket” are replaced with metal and plastic, its a total hip replacement. Depending on activity level, orthopedic doctors recommend either a hip replacement, or a half hip replacement. 10 years ago the “hemi” was the mainstay of treatment, however, new studies are showing that people receiving a complete hip replacements have better mobility and less pain with walking. In elderly that are minimally active, its not a big deal to have minor discomfort getting around and it certainly it outweights the risk of the bigger total hip replacement surgery. However, our elderly are healthier and more active that ever, and this means that many of them will not be satisfied with a procedure that can leaves them with some residual discomfort. In such cases maybe a total hip replacement is a better option. The bigger message is that there are multiple treatment options and all are successful in the correct situation. The ultimate decision must be made after a conversation between the patient, their family, and the doctor.
The Intertrochanteric hip fracture (slang “Intertroc” by orthopedic surgeons) occur with the same frequency and in the same population as the femoral neck fractures. An Intertroc fracture occurs outside of the hip joint (they are still called hip fractures because they are still close to the joint). Every joint is surrounded by a capsule which is great for the cartilage because it holds the joint fluid (which is like motor oil) and keeps the cartilage lubricated. However, this joint fluid gets in the way of bone healing, and therefore, fractures that occur within the capsule don’t heal well (think femoral neck fracture). Intertroc fractures are outside the capsule and have better blood supply, and therefore they heal better than femoral neck fractures. There is a thick portion of bone within this region called the “calcar” and it acts like a buttress (it gives a lot of support to our hip which must hold up our whole body weight). If the fracture line goes into this part of the bone, the injury is considered unstable, and may heal more slowly.
All of these fractures should be treated with surgery, which uses hardware (a pin and screw, or a plate and screw), to realign the bone while it heals. Surgery also enables patients to begin walking on the broken leg as soon as its fixed.
The Subtrochanteric fracture (called a “Subtroc” by surgeons) occurs less frequently than the other hip fractures and it is often seen in people that taking medication for osteoporosis. The bisphosphonate medication slows osteoporosis but causes the bone in this “subtroc” region to look a little irregular and probably not as good at withstanding stress. It’s a little bit of robbing Peter to pay Paul (the medicine reduces the risk of fracture in some parts of your body but increases the risk in others). These fractures require surgery to heal because the bone fragments are almost always pulled apart by our thigh muscles. Surgery will realign the bones and then use an intramedullary nail (goes down the center of the bone) to hold everything in place while it heals. These fractures heal better than femoral neck fractures but worse than intertroc fractures. Again its all about the blood supply. Patients can start walking on the injured leg as soon as its been surgically repaired.
What is the long term outcome?
How well does it heal and what complications can occur?
After the surgery patients can walk on their hip as tolerated, 90% will heal, and the rate of disrupted blood supply causing bone to die, is between 1-20%. 15% of nondisplaced, and 25% of displaced fractures develop avn. This is more important in younger patients because it increases their risk for early arthritis and need for joint replacement at an age that tests the longevity of current joint replacements. Its less of an issue in elderly because they can often decrease their activity if this complication occurs and they will continue to live a good life without further surgery (some show that ¼ have no symptoms, while about ½ have some symptoms but an acceptable level of disability). In the remaining 1/4 it may become painful and would require a hip replacement, which is common place in people at that age and would be expected to do very well. In displaced fractures of the femoral neck, we are very concerned for AVN (disruption of blood supply), in fact it occurs more often than not. However, in patients 60 years old, we still want to take the chance of fixing it and preserving the bone, with the understanding that theres a good chance the surgery wont work and the patient will have to return for a hip replacement.
The biggest problem with hip fractures is there is a high rate of mortality (death) following this fracture. Many doctors believe that most people who get this injury are frail and sick to begin with, and once this injury occurs, its just too much for their body to recover from. Its sort of a straw that breaks the camels back. Theres about a 30% 1 year mortality associated with this fracture, about 15% hospital mortality. This mortality rate is 4-5x higher than non-hip fracture people of the same age. Some studies show that hip fractures which are not treated have 1 year mortality rates around 90% due to the very high incidence of pneumonia, bed sores, blood clots and other issues that are likely to develop when someone of that age is bed bound for a prolonged amount of time.
Reference
INTERTROCH
1. Lindskog DM, Baumgaertner MR. Unstable intertrochanteric hip fractures in the elderly. JAAOS 2004; 12(3): 179-90. see article. review treatment options.
2. Baumgaertner MR, Solberg BD. Awareness of tip-apex distance reduces failure of fixation of trochanteric fractures of the hip. JBJS Br. 1997; 79(6): 969-71. see article. classic showing <25 mm on combo ap lateral tip apex reduces screw cut out.
FEM NECK
1. Blomfeldt R et al. Displaced femoral neck fracture: comparison of primary total hip replacement with secondary replacement after failed internal fixation: a 2-year follow up of 84 patients Acta Orthop 2006; 77: 638-643. see article. primary THA does better. high risk failed orif.
2. Keating JF et al. Randomized comparison of reduction and fixation, bipolar hemiarthroplasty, and total hip arthroplasty. Treatment of displaced intracapsular hip fractures in healthy older patients. JBJS 2006; 88(2): 249-60. see article. 207 pts. 40% reoperation with orif, 5% w. hemi, 9% with tha.
3. Blomfeldt R et al. A randomized controlled trial comparing bipolar heiarthroplasty with total hip replacement for displaced intracapsular fractures of the femoral neck in elderly patients. JBJS Br 2007; 89: 160-165. see article. classic. no inc complications with THA, better 1 yr harris hip scores.
4. Moran CG et al. Early mortality after hip fracture: is delay before surgery important? JBJS 2005; 87(3): 483-9. see article. 2.5 inc 30 day mortality of treatment delayed due to acute medical comorbidity (17% 30 day). no difference up to 4 days delay, if >4 days, inc 30 day (10% vs 7%) and 1 yr mortality (30%).
5. Booth KC et al. Femoral neck fracture fixation: a biomechanical study of two cannulated screw placement techniques. Orthopedics 1998; 21(11): 1173-6. see article. inverted triange, 3 mm from cortex is strongest for cann screw fixation.
6. Haidukewych GJ et al. Operative treatment of femoral neck fractures in patients between the ages of fifteen and fifty years. JBJS 2004; 86(8): 1711-6. see article. only 15% req. conversion to THA for AVN, but no impact of timing, anatomic reduction, initial displacement are most important.
SUBTROCH
1. Goh SK et al. Subtrochanteric insufficiency fractures in patients on alendronate therapy: a caution. JBJS Br 2007; 89(3): 349-53. see article. alondronate and others inc risk subtroch.
2. Robinson CM et al. Trochanteric-entry long cephalomedullary nailing of subtrochanteric fractures casued by low-energy trauma. JBJS 2005; 87(10): 2217-26. see article. gamma nail (long cephomed nail) is good treatment.