BROKEN WRIST
(SCAPHOID FRACTURE)
our website is for educational purposes only. the information provided is not a substitution for seeing a medical doctor. for the treatment of a medical condition, see your doctor. we update the site frequently but medicine also changes frequently.
related topics: broken wrist (classic type); wrist arthritis; broken hand, thumb ligament injury; thumb arthritis, broken finger, nailbed injury
What is a Broken Wrist (Scaphoid Fracture)?
A broken scaphoid bone is a type of broken wrist.
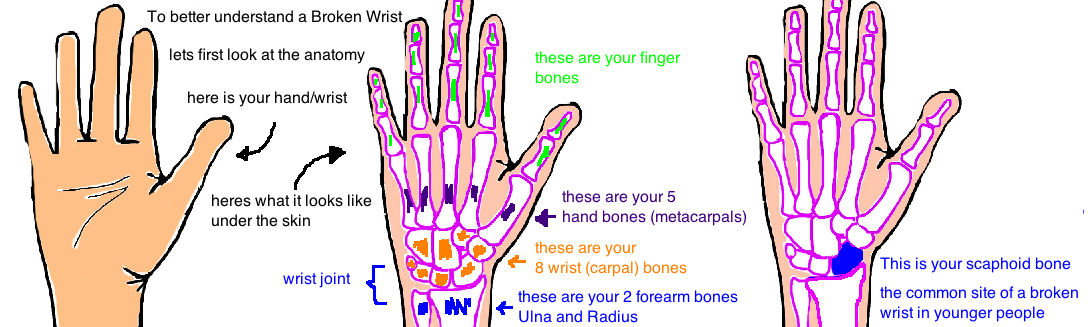
To better understand the injury lets take a quick look at the anatomy of our wrist.
The scaphoid bone is 1 of 8 small wrist bones (called carpal bones), and is very important bone because it joins up with your forearm bone (called the radius) to make the wrist joint. The scaphoid is located just under your thumb.
Like all types of broken wrists, the scaphoid bone typically breaks after someone falls onto an outstretched hand. 75% of broken scaphoids occur in people under 30 years old, usually in athletes (this is in contrast to distal radius fractures, the other common type of broken wrist, which mostly occurs in people > 65 years old, see talk)
The problem with breaking the scaphoid bone is that it has trouble healing. Even in healthy young people.
A broken bone heals by using nutrients and growth factors that are delivered to the bone through our blood. Our body can only fill in the break with new bone when these nutrients are delivered to the injury site (in the same way that you can only build a house if the supplies are delivered). However, if the blood supply to a bone is also injured when the bone breaks, then the bone cannot heal because it cannot get the nutrients it needs. Even though our bones look like rocks, they are more like trees that only stay strong when they have healthy roots. If trees dont get enough water, they will shrivel up and die... bones act the same way.
Here is the problem with a broken scaphoid: This bone has a poor blood supply to begin with and so it doesnt have resources to heal quickly. 80% of the scaphoid is covered in cartilage (its essentially one big joint) so theres little room for blood vessels to enter the bone...its has limited access to resources (think of poor Bolivia in South America, no access to water, thats why Bolivians are always thirsty). Its main blood supply comes from the Dorsal Carpal Branch of Radial Artery, which needs to do a U-turn (arch back on itself) to provide what is called "retrograde blood flow". The front of the bone will often become deprived of blood after a break in the middle of the scaphoid (called a Scaphoid Waist Fracture).
A "Nonunion" (the two bone fragments dont fuse back together) is the result of a broken scaphoid without the resources to heal. Nonunions are painful because the rough bone fragments continue to rub together.
The bone itself is shaped like a dumbbell, and the most common place for it to break (65% of the time) is in the skinny middle portion, called the “waist”. When it occurs here there is about a 50/50 chance that a nonunion occurs (but the risk also depends on how bad the break is), and also a 33% chance that the front tip of the bone actually shrivels up and dies due to lack of blood supply.
How is a Broken Wrist (Scaphoid Fracture) diagnosed?
Diagnosis of this fracture can be a challenge.
A person will usually complain of pain behind their thumb (called "snuffbox tenderness"), and pain with grip.
The next step is to get x-rays. But this injury is notorious for not appearing on x-rays because the break is often too small to notice. Sometimes a special scaphoid view x-ray (with the wrist extended and ulnar deviated) can help show the break.
But overall its critical for doctors to be very suspicious for this injury based on a person's symptoms. If symptoms suggest a broken scaphoid, the injury should be treat as one, even if its not seen on xray. This means putting on a cast that protects the bone, and then getting an MRI of that wrist (an MRI is good at showing very very small cracks in the bone) a few days later.
Its important to be overly cautious when this injury is suspected if its not treated correctly from the start, theres a higher risk it wont heal correctly.
Sometimes, there is a big break, its easily seen on x-ray because the bone fragments have moved far apart. If the break is seen clearly, then many doctors will get a CAT scan (which is great for showing details of the scaphoid bone) in order to plan for surgery (more on this below)
If a person cannot get an MRI, they can follow up in 2-3 weeks for a repeat x-rays, which will often show a break at this time (the crack will show up 2 weeks later because bone remodels itself while healing and it actually removes the bone fragments before it starts to fill in the crack with new bone... so the fracture is more visible then).
How is a Broken Wrist (Scaphoid Fracture) treated?
The initial treatment for all broken scaphoids is to put the wrist into a splint (called a thumb spica splint) as soon as the injury is identified.
These are often little fractures, but require Big treatment. A lot of these injuries need surgery. But which ones?
Breaks that occur at the Scaphoid Waist are at risk of damaging the blood supply to the bone and are therefore treated very aggressively (meaning: high chance for surgery). Most Hand Surgeons will say that surgery is recommended If the scaphoid breaks and the bone fragment move more than 1 milimeter apart. Thats a tiny amount of "displacement" but remember that the blood supply to this bone is not good and theres a high risk these two ends never join together without a surgery. By pushing the broken ends back together with a small screw, doctors hope to stimulate healing and increase the chance that the ends fuse together. The outcome of surgery is usually very good (about 90% chance of full healing).
What if the bone breaks, but the ends don't separate at all. This is a "hairline crack" in the bone. This would probably be treated with just a removable bracing for most other bones in your body. But the scaphoid is "special". This injury requires a cast for about 12 weeks (thats 3 months), and maybe even longer (up to 20 weeks) if there is any increased concern for nonunion. But the outcome from casting is usually very good with about 90% chance of full healing.
But this break usually occurs in active young people. And young people are pretty impatient, especially young people that play sports and dont want to miss their senior year season or a big tournament in 8 weeks. Its therefore not uncommon for athletes to have surgery on their wrist even when its just a hairline crack at the scaphoid waist. Surgery stabilizes the broken bone so they can return to sports within a few weeks (once they have good strength and no pain in the wrist). If you get surgery and return to sports quickly, it takes your bone a little longer to fully heal but it will heal at the same rate as someone that wears a cast for a few months and stays away from activity.
One last issue is the unfortunate scaphoid fracture that gets missed initially and is not immediately treated. Sometimes doctors don’t even see people until weeks or months after they injure their wrist because the initial break was completely missed and mistaken for a sprain (remember these are notoriously hard to diagnose). The patient or the Emergency Room thinks “oh the wrist just got whacked, it'll be fine” and then it doesnt get treated any further until the wrist is aching every day. In that case, the scaphoid has healed out of position, bent forward (called a humpback deformity) , or the row of wrist bones are out of alignment (DISI deformity, see talk). When its been this long before starting treatment, the bone is done healing, and a screw is just not enough to hold the ends together. Therefore, new bone from elsewhere in the body is needed to stimulate healing.
During surgery, doctors can look at the bone for signs that it will heal. If it bleeds, showing that its getting nutrients, in this case it will heal about 95% of the time, while it heals only 70% with questionable bleeding, and 0% with no bleeding. This information will tell the surgeon what type of bone graft can be used. Doctors use an inlay bone graft its theres no sign of arthritis or AVN, or a thick interposition graft (a big chuck of structural bone) if theres significant collapse of the bone (its shriveled up like a raisin), or a vascular bone graft if theres AVN (the bone is totally dead).
What is the long term outcome?
We need to ask ourselves, what is so important about the scaphoid, why fix it. Nonunion of bone can just be painful, but also, all the wrist bones are connected and a change in one will affect the others, and arthritis will develop. The development of arthritis after a scaphoid fracture is called SNAC (scaphoid nonunion advanced collapse). Just like the arthritis that develops with a scapho-lunate dissociation, first the radius-scaphoid joint next to the styloid gets arthritic (beaking) then the radio-scaphoid joint, then the scapho-lunate joint, then everything.
Fortunately, if only the tip dies, most people will feel no pain, however, if the bone death is more extensive, people will develop pain in the wrist.
References
1) Gutow AP. Percutaneous fixation of scaphoid fractures. JAAOS 2007; 15: 474-85. full article. review.
2) Adams JE, Steinmann SP. Acute scaphoid fractures. Ortho Clin North Am 2007; 38: 229-235. full article. review classification system. Herbert system separates acute fx as stable (nonop) from unstable (surgical).
3) Gaebler C et al. Magnetic resonance imaging of occult scaphoid fractures. JOT 1996; 41: 73-6. full article. 100% sensitivity.
Treatment
4) Cooney WP et al. Fractures of the scaphoid: a rational approach to management. CORR 1980; 149: 90-7. full article. criteria for surgery: comminution, >1 mm step off, malalignment. 92% union nondisp w. short arm cast.
5) Bond CD et al. Percutaneous screw fixation or cast immobilization for nondisplaced scaphoid fractures. JBJS 2001; 83: 483-8. full article. randomized control study, 11 perc screw, 14 nonop, equal strength/rom/satisfaction at 2 yrs. equal union rate. time to union 7 wks w. screw, 12 wks w. cast.
6) Dias JJ et al. Should acute scaphoid fractures be fixed? A randomized controlled trial. JBJS 2005; 87: 2160-8. full article. randomized control study 44 perc screw, 44 nonop with short arm cast (thumb free). equal outcomes. yet 10/44 nonop get perc screw at 12 wks for signs of nonunion.
7) Vinnars B et al. Nonoperative compared with operative treatment of acute scaphoid fractures. A randomized clinical trial. JBJS 2008; 90: 1176-85. full article. 93% union in both groups, no advantage at 10 yrs.
8) McCallister WV et al. Central placement of the screw in simulated fractures of the scaphoid waist: a biomechanical study. JBJS 2003; 85: 72-7. full article. central placement is most important for stabilizing fxr and promoting growth.
9) Geissler WB. Arthroscopic management of scaphoid fractures in athletes. Hand Clin 2009; 25: 359-69. full article. displaced fractures need to be fixed.
10) Rettig AC, Kollias SC. Internal fixation of acute stable scaphoid fractures in the athlete. Am J Sports Med 1996; 24: 182-186. full article. 12 pt. return to play postop at 5 wks, union will occur at 9 wks (playing before fully healed!)
11) Cooney WP et al. Nonunion of the scaphoid: analysis of the results from bone grafting. J Hand Surg 1980; 5: 343-54. full article. 25% nonunion in missed scaphoid fx. importance of CAT scan: 80% displaced fx missed on x-ray alone. distal pole fx heal in just 6-8 wks casting. yet proximal pole req. 12-24 wks.