BROKEN FINGER
(PHALANX FRACTURE)
our website is for educational purposes only. the information provided is not a substitution for seeing a medical doctor. for the treatment of a medical condition, see your doctor. we update the site frequently but medicine also changes frequently.
related topics: nailbed injury, broken thumb, thumb ligament injury, broken wrist, mallet finger, jersey finger
What is a Broken Finger (Phalanx Fracture)?
A broken finger (also known as a phalanx fracture) is a very common hand injury. In fact, its the most common bone to break in your whole body, and it represents almost 10% of all broken bones.
In people under 30 years old, fingers are usually broken during sports; and for people between 30-70 years old, fingers are typically broken from a machine or work related accident, and in people older than 70, its usually broken during a fall.
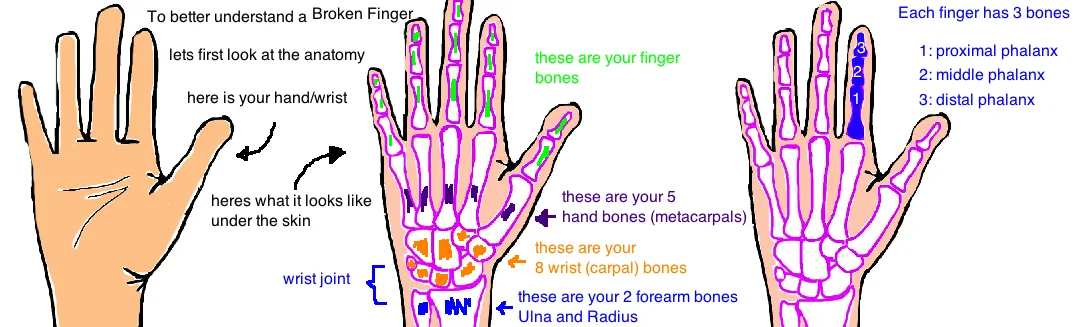
Lets quickly review the anatomy of our hand.
Our wrist bones are called carpal bones (we have 8), our hand bones are called metacarpals (we have 5, one for each finger), and our finger bones are called phalanx bones. Each finger has 3 phalanx bones. The first bone in your finger is called the proximal phalanx, the middle finger bone is called the middle phalanx, and the finger tip bone is called the distal phalanx.
In this talk we will look at the diagnosis and treatment of a broken proximal or middle phalanx.
A broken distal phalanx (the tip of the finger) usually occurs when your finger gets crushed (like caught in a door) and this is called a "Tuft Fracture" and is discussed in a separate section because its so common (see talk).
How is a Broken Finger (Phalanx Fracture) diagnosed?
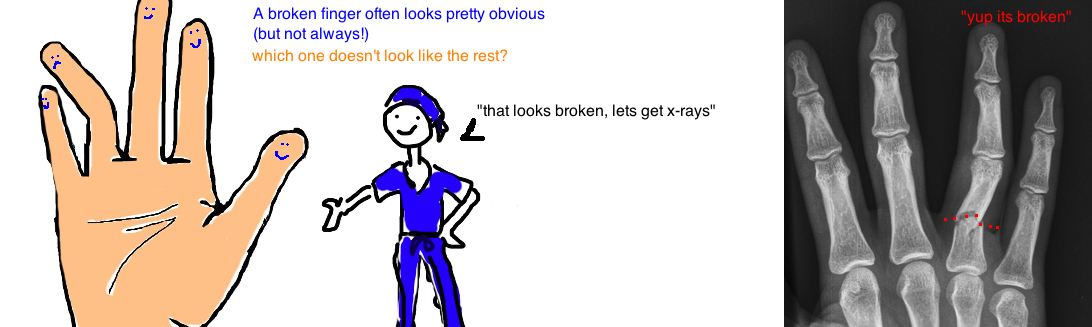
A broken finger is suspected when someone reports injuring their finger and is experiencing significant pain and swelling. A finger bent out of place is a pretty good indication that the finger is either broken or dislocated (or both). The inability to bend your finger due to pain is also suggestive of a break. If your doctor suspects a broken finger, the next step is to get an x-ray.
An x-ray of the injured finger is a good way to diagnose a broken finger, and usually its the only tested needed for diagnosis.
X-rays of the broken finger are then used to guide treatment.
How is a Broken Finger (Phalanx Fracture) treated?
All broken fingers are not equal, some need surgery and some just need buddy tape. So how do doctors decide? The first step is to look at the pattern of the break. Looking at the x-rays doctors determine 1) if it enters into the joint (aka knuckle, where the two finger bones come together and allow your finger to bend), 2) if its broken in multiple places; 3) if the bone fragments have moved out of position.
A break in the finger bone that stays away from the joint ("extra-articular") is usually treated by simply buddy taping it to the neighboring finger for about 3 weeks (longer immobilization has an increased risk for causing long-term finger stiffness). Buddy tape works well as long as the broken bone is in normal or near normal alignment (this shows that its stable...low risk that it will get worse). If the bone is broken in only one place and its bent less than 10 degrees and it hasn't shortened or rotated, then its stable. Buddy tape is great because recruits your neighboring finger as a splint to give protection and stability to the injured finger, while also allowing your finger to move a little bit so that it doesnt get too stiff (stiffness is a real concern with finger injuries, more on that later).
However, if the finger is broken into multiple pieces or if the crack in the bone enters one of the knuckle joints ("intra-articular") or if the bone fragment has moved significantly out of position, then surgery is often recommended. If the finger bone shortens more than 2 milimeters or is bent over 10 degrees, an "extensor lag" will develop, which means that you cannot fully straighten that finger (the biomechanics are changed).
Breaks that go into the finger joint (called "Condyle Fractures") are unstable even if it looks like a tiny hairline crack ("nondisplaced"). They typically require surgery . A "Pilon Fracture" at the base of the middle phalanx is another common break that involves the joint, its usually accompanied by cartilage injury, and frequently needs surgery to restore the joint surface.
The goal of surgery is to get the broken bone to normal alignment, and then hold the bone in alignment while it heals. Surgery typically involves using a few tiny screws, a small metal plate, or two pins to hold the broken bone fragments in good alignment. The metal gives extra stability while the bone heals. Many x-ray pictures are taken during surgery to ensure that the bone is straight. If screws are used, they stay in the bone forever while pins are removed after 3-4 weeks. One of the biggest advantages to surgery is that finger motion can be started almost immediately and this will really help to reduce the risk of stiffness.
In some cases, the finger is bent back way too far, and the first bone not only breaks but the second bone dislocates (meaning the knuckle joint separates). This injury is called a Fracture-Dislocation. It occurs because the break enters the knuckle joint and causes instability. The first goal is to put the finger back in place, and the next goal is to position the finger so that it stays in place while it heals. If the fragment of bone is less than 40% of the joint surface, it will probably heal with the finger splinted in a bent position (using an extension-block splint). If the bone fragment involves more than 40% of the joint, it will probably require surgery to restore stability to the knuckle.
Overall, the goal of treatment is to get the broken finger in good alignment so that it functions well. The broken bone must be stable to heal, so it can be treated with a splint or buddy tape if the break isnt so bad, or it can be treated with surgery if its really smashed and needs pins or screws to give extra stability.
What is the long term outcome?
Finger stiffness is a major concern after a broken finger.
A crack that goes into a knuckle joint definitely puts people at increased risk for stiffness. But other breaks that require your finger to be immobilized for a few weeks also dramatically increase the risk for stiffness. Buddy tape is a great treatment because people can start moving their fingers immediately, But in cases that need a more rigid splint (or pins for surgery), its critical to start moving the finger within 4 weeks or else the risk of permanent stiffness approaches 40%.
This is why its so important to talk with your doctors about the pros-and-cons of treatment options so that you can figure out the best thing for you.
References
1. Henry MH. Fractures of the proximal phanalx and metacarpals in the hand: preferred methods of stabilization. JAA)S 2008; 16: 586-95. see article. review.
2. Kozin SH et al. Operative Treatment of Metacarpal and Phalangeal Shaft Fractures. JAAOS 2000; 8: 111-121. full article. review
3. Ebinger T, Erhard N, Kinzl L, Mentzel M: Dynamic treatment of displaced proximal phalangeal fractures. J Hand Surg 1999; 24:1254-1262. see article. 48 displaced prox phalanx fx, all healed with nonop rx. remove hard splint/cast by 3 wks, buddy tape.
3. Dabezies EJ, Schutte JP: Fixation of metacarpal and phalangeal fractures with miniature plates and screws. J Hand Surg 1986;11:283–288. see article. 90% normal ROM in 25 MC and 27 phalanx fx after ORIF. good outcome data.
4. Page SM, Stern PJ. Complications and range of motion following plate fixation of metacarpal and phalangeal fractures. J Hand Surg 1998;23: 827–832. see article. 100 MC, 100 phalanx fx after ORIF, only 50% got >200 deg motion. mixed outcome data.
5. Diwaker HN, Stothard J. The role of internal fixation in closed fractures of the proximal phalanges and metacarpals in adults. J Hand Surg Br 1986; 11:103–108. see article. compared 50 k-wire and orif vs 50 nonop rx. orif best motion (80% got 200 deg motion) vs only 50% in k-wire, nonop.
6. Green DP, Anderson JR: Closed reduction and percutaneous pin fixation of fractured phalanges. JBJS 1973;55:1651–1654. see article. perc pinning technique.