NECK ARTHRITIS - CERVICAL MYELOPATHY
our website is for educational purposes only. the information provided is not a substitution for seeing a medical doctor. for the treatment of a medical condition, see your doctor. we update the site frequently but medicine also changes frequently. thus the information on this site may not be current or accurate.
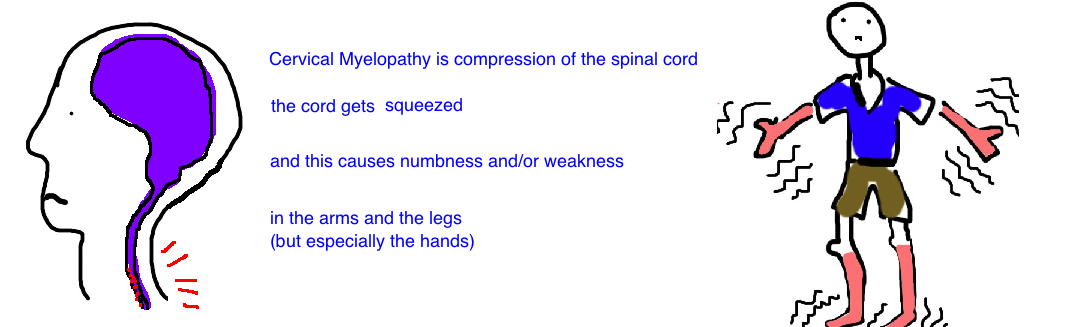
What is Cervical Myelopathy?
Myelopathy is a spine condition that results in clumsy hands and an unsteady gait. Excessive pressure on the spinal cord in the neck prevents the nerves from functioning properly.
A person's arms and legs do not function properly because the spinal cord itself is compressed. The most common cause of cord compression is from degenerative arthritis which narrows the space that the spinal cord travels in. But there are many other things that can narrow this space, including a traumatic injury (see the burst fracture talk), a herniated disc, a tumor, or a bacterial abscess. But the most common by far is gradual degeneration of the vertebrae.
Additionally, our neck is normally not completely straight but has a slight backward bend to it, called lordosis. However, as our neck becomes arthritic this curve flattens out (our neck starts to bend forward), and this change in architecture causes the spinal cord to press up against the front of the bones, and this adds to the compression.
In contrast, Radiculopathy (which is pain that radiates down the arm...see talk) is caused by compression of a spinal nerve. Myelopathy is caused by compression of the spinal cord.
Remember that the spinal cord is the mother of all nerves. It travels from your brain to your lower back, and along the way, smaller nerves (called spinal nerves) branch off. These exit the spine and travel down your arms and legs, branching off along the way to form all the nerves in your body. So when the spinal cord itself is compressed, a lot of problems can occur. This is what we will discuss.
How is Cervical Myelopathy diagnosed?
People come into the office complaining of clumsiness of their hands and/or difficulty walking and feeling unstable on their feet.
A lot of times people don’t have any complaints of pain.
Over time, symptoms typically get worsen. This worsening of symptoms occurs in a step-like pattern, meaning there are periods of stable symptoms followed by episodes of deterioration, and then another period of stable symptoms.
X-rays will show degenerative changes to the vertebrae, and may also show a flattening out of the normal neck curvature.
Doctors can also measure the width of the spinal canal (the space in the vertebral bones that the cord travels through). it is normally about 17 mm wide, and if its less than 13 mm, its considered abnormally narrow. However, a lot of changes seen on x-ray are not specific to the symptoms a person is having. We know this because about 70% of people over 70 years old have signs of a degenerative spine, however most of them dont have symptoms of cervical myelopathy.
An MRI is probably the most useful test to look for injury to the spinal cord itself, and also to look at areas of spinal cord narrowing or low amounts of cerebral spinal fluid which normally bathes the spinal cord and helps provide nutrition. The results of x-rays and MRIs can be used in combination with a good neurologic exam to determine the location along the spine thats causing the symptoms.
How is Cervical Myelopathy treated?
If left alone, this condition slowly progresses with time, and rarely improves without surgery.
The mainstay of treatment in someone presenting with gait symptoms, or progressive clumsiness of their hands, is to perform surgery to decompress the spinal cord.
Particularly when people have problems with walking, surgery is a necessary intervention. The surgery performed is called an anterior cervical discectomy and fusion. The surgeon approaches the spine by making a small incision in the front of the neck, removes the vertebral disk and the bone that is narrowing the spinal canal, and fuses two or three of the vertebral bones in a position that gives the spinal cord more room.
What is the long term outcome?
Current studies show that surgery leads to about 80% of people reporting improved pain and 90% report improve neurologic symptoms. But its important to remember that the best predictor of outcome is the patients condition before surgery.
People that show the best success are those whose symptoms are identified early in their course, and treated quickly. If someone had significant leg weakness for months before surgery and an MRI showing significant spinal cord injury, their chances of a dramatic response to surgery are lower than someone who underwent surgery after a few weeks of leg weakness and a MRI showing mild spinal cord injury.