BROKEN FOOT
(TALUS FRACTURE)
our website is for educational purposes only. the information provided is not a substitution for seeing a medical doctor. for the treatment of a medical condition, see your doctor. we update the site frequently but medicine also changes frequently.
related talks: broken ankle (classic type); broken foot (jones fracture); broken foot (lisfranc type fracture); broken heel bone; low ankle sprain; high ankle sprain
What is a Talus Fracture?
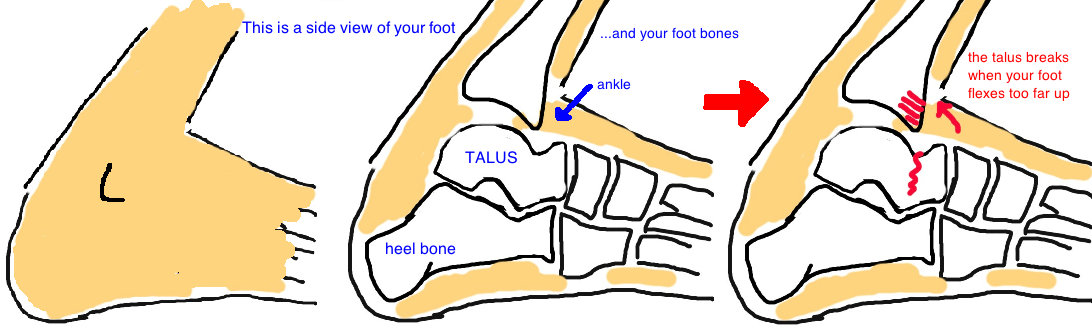
The talus is a bone in the middle of the foot that makes up part of the ankle joint.
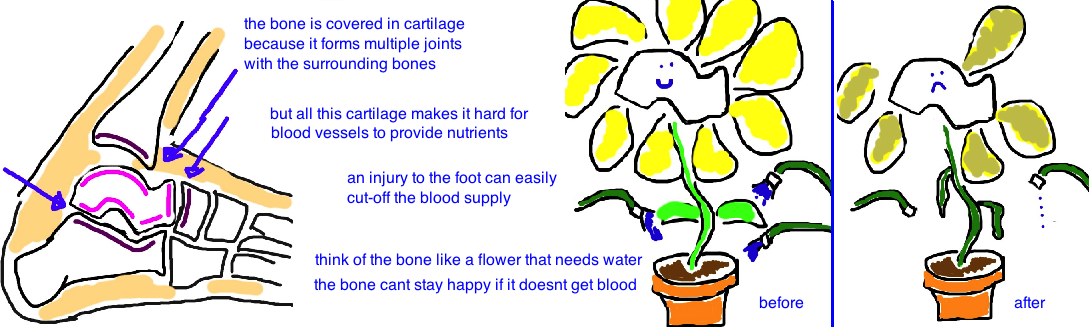
To better understand a talus injury, lets quickly review the anatomy of our foot and ankle. The ankle joint consists of three bones: the tibia and fibula (both leg bones) and the talus (a foot bone). The talus is almost entirely covered in cartilage (well actually about 50%, but that’s a lot for a bone). Because all of our body weight is transmitted through this relatively small bone, its large cartilage surface area helps to distribute stress of walking and running. Remember, cartilage is our body's natural shock absorber. Our talus does such a good job at tolerating stress, you almost never hear of natural arthritis developing in the ankle. You've probably know friends, family or neighbors that need a hip or knee replacement due to severe arthritis in those joints, but when have you heard of a total ankle replacement? Probably never (maybe you have... but its uncommon). Usually if arthritis occurs, its due to a prior injury that causes post-traumatic arthritis.
The talus can fracture after a high-energy injury like a car accident or falling from a height when the foot is forcefully flexed upward (dorsiflexed) causing it to push against the tibia. Its uncommon for the talus to break after a twisting injury, which usually causes a classic "broken ankle".
The talus looks like a dumbbell, it has a large round part that forms the ankle (aka talar body) and another large round part that meets up with the mid foot (aka the talar head), and then theres a thin “neck” which connects the two. This neck is the part that breaks in 50% of talar injuries.
A Talar Neck Fracture can be problematic because the artery that provides blood (meaning nutrients) to the bone can be damaged, creating problems for healing. Oftentimes, the talus bone will become dislocated from the ankle joint, or the subtalar joint in addition to being fractured.
How is a Talus Fracture diagnosed?
A fracture to the talus bone is suspected based on the location of pain and swelling at the top of the foot, near the ankle. The mechanism of injury (like a fall of a ladder) also suggests a more severe injury like a broken talus (or even a broken heel bone, see talk).
Doctors will order x-rays to diagnose the injury and will also tell doctors about the severity of injury. Many times a CAT scan (which gives 3D x-ray pictures of the bones) will also be performed to give an even better look at things.
Diagnosing the break, and its severity will determine the best treatment.
How is a Talus Fracture treated?
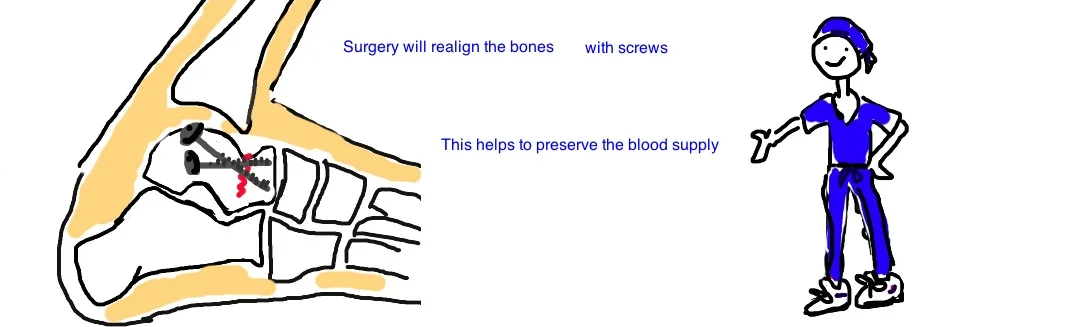
Surgery is often required to prevent permanent deformity and to minimize the risk of post-traumatic arthritis.
Surgery also needs to be performed as soon as possible. Good outcome from this injury depends on the blood supply. Bone needs nutrients to heal, however, the blood supply is frequently disrupted in talar neck fractures. Therefore, it is critical to realign the talus to maximize the chance that arteries are not kinked, so that nutrients are delivered to the bone allowing it to heal.
Surgery uses small screws to hold the broken fragments together. The surgeons will make incisions on both sides of the foot.
The talus is part of multiple joints in the foot (talonavicular joint, the subtalar joint, and the ankle joint). Fractures that enter the joint (which is common) need to be nearly perfectly realigned to minimize the risk of arthritis (if the cartilage is uneven due to a crack in the bone, the cartilage will wear out quickly due to the changes in contact pressures.
Nonsurgical treatment is only recommended if there is a hairline crack without movement of the bone fragments (this also suggests that the artery was not damaged). In such cases the foot will be put into a cast and kept immobilized (no standing on the foot for 6-8 weeks!).
What is the long term outcome?
Outcome of the injury depends on the severity of the initial fracture, and the preservation of blood flow to the bone. A small crack in the talar neck carries about a 10% risk, while a fracture plus a subtalar dislocation carries a 30% risk. A fracture plus a dislocation from the ankle joint carries a 90% risk. It is a major concern because the bone can shift into abnormal alignment (called varus malunion) when its weakened by poor blood flow. The malignment that results limits foot motion and lead to premature arthritis if its not corrected with other surgical procedures (called an "opening wedge osteotomy", or a triple arthrodesis, aka ankle fusion).
Even with early repair of the broken talus, only about 60% of these injuries have good to excellent outcomes.
X-rays taken around 6 weeks after the injury can monitor the injured foot for signs of weak bone due to poor blood flow (doctors look for signs signs of sclerosis on x-ray which means the unhealthy bone thickens).
The other major complication is post-traumatic arthritis, particularly in the subtalar joint (the talocalcaneal joint), and the risk is about 50% (but can approach 90% in bad fractures). Surgery minimizes this risk by returning the bone to its normal alignment, but sometimes the cartilage damage from the injury is irreversible and doctors have still not developed a good way to treat cartilage injury.
References
1) Canale ST, Kelly FB Jr. Fractures of the neck of the talus. Long-term evaluation of seventy-one cases. JBJS 1978; 60: 143-56. full article. ok outcomes, complications avn risk based on severity.
2) Lindvall E et al. Open reduction and stable fixation of isolated, displaced talar neck and body fractures. JBJS 2004; 86: 2229-34. full article. outcome displaced fx rx orif.
3) Vallier HA et al. Talar neck fractures: results and outcomes. JBJS 2004; 86: 1616-24. full article. risk avn, no effect delay sx on avn risk.
4) Vallier HA et al. A new look at the Hawkins Classification for talar neck fractures: which features of injury and treatment are predictive of osteonecrosis? JBJS 2014; 96: 192-7. full article. avn risk factors.
5) Sanders DW et al. Functional outcomes following displaced talar neck fractures. J Ortho Trauma 2004; 18: 265-70. full article.
6) Herscovici D Jr et al. Avoiding complications in the treatment of pronation-external rotation ankle fractures, syndesmotic injuries, and talar neck fractures. JBJS 2008; 90: 898-908. full article. reviewing ankle injuries.
7) Tezval M et al. Prognostic reliability of the Hawkins sign in fractures of the talus. J Ortho Trauma 2007; 21: 538-543. full article. good at predicting vascularity post-injury.
8) Fortin PT, Balazsy JE. Talus fractures: evaluation and treatment. JAAOS 2001; 9:114-27. full article. review.
9) Hawkins LG. Fractures of the neck of the talus. JBJS 1970; 52: 991-1002. full article. classic paper.
10) DiGiovanni CW et al. Proximity of the lateral talar process to the lateral stabilizing ligaments of the ankle and subtalar joint. Foot Ankle Int 2007; 28: 175-8. full article. other talus fx.