FINGER & FINGER NAIL INFECTIONS
our website is for educational purposes only. the information provided is not a substitution for seeing a medical doctor. for the treatment of a medical condition, see your doctor. we update the site frequently but medicine also changes frequently. thus the information on this site may not be current or accurate.
Types of Finger Infections
There are many types of infections that can occur in the fingers and hand. We will talk about the most common types which include: 1) hand cellulitis; 2) nail infections ("paronychia"), 3) finger pulp infection ("felon"), 4) bite infection; 5) flexor tenosynovitis; 6) fingernail fungal infection.
Cellulitis of the Hand
One of the most common hand infections is Cellulitis (an infection of the skin) which causes the hand to become red, swollen and painful.
There are 2 types of bacteria that are the main culprits for this infection:
1) staphlacoccus aureus (one strain is known as MRSA: methicillin-resistant staph aureus, and it often makes news because it is resistant to many antibiotics).
Staph has the tendency to form abscesses (walled off collections of pus) which may require surgery to open ("lancing the bump"). Surgery is needed to treat an abscess because it seals itself off from the rest of the body, preventing antibiotics from reaching it. MRSA, that particularly nasty version, often has a classic appearing abscess, which is a red pimple with a black center (it looks similar to a spider bite). Typical antibiotics for treatment include antibiotics like Clindamycin or Bactrim or Levaquin.
2) Streptococcus pyogenes.
Strep causes red streaking up toward the shoulder, it doesn’t cause pus to form, and it rarely requires surgical treatment. It mainly just needs antibiotics to treat (penicillin or 1st gen cephalosporins). Although this bacteria can make headlines as a "flesh eating bacteria" (aka Necrotizing Fascitis) because very very rare cases (usually in diabetics or people with a weakened immune system) can spread rapidly through the body (in a matter of hours or days if left untreated).
Finger nail abscess (Paronychia)
A Paronychia is an abscess around the finger nail. Its common in women that get a manicure at a dirty beauty parlor, or from other issues, like people that bite their nails.
The area of skin on the side of the nail is called the parinychium, while the skin covering the base of the nail is the eponychium (this part of the skin covers the germinal nail matrix, which allows nails to grow).
These abscesses can be very painful. Sometimes they can be treated with warm soaks, which causes the abscess to burst, and this relieves the pain by decompressing the abscess. Sometimes these need to be lanced if the soaks fail.
If the abscess requires lancing (medically termed "incision and drainage" or "I&D"), it should be performed by a health care professional because if performed incorrectly, an injury to the nail bed may cause abnormal finger nail growth.
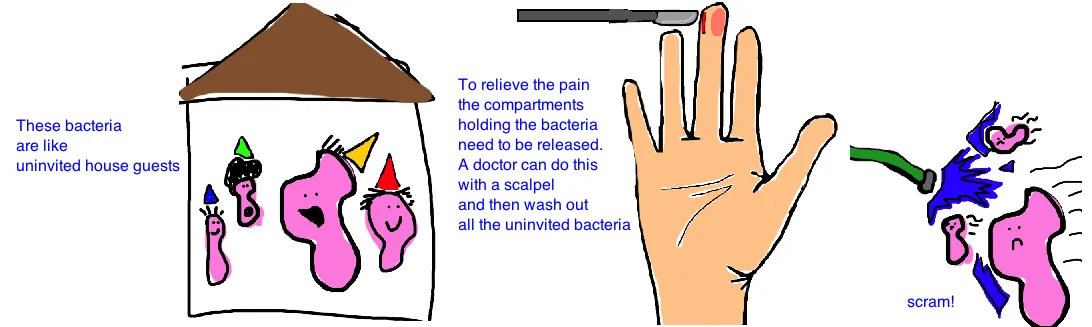
The reason for cutting the abscess open is that we want to push the bacteria out of the body. The bacteria wants to stay: they wall themselves off, and prevent antibiotics from entering their space). Think of bacteria as a party guest that has overstayed their welcome...they've invaded your house and now locked themselves in the guest bedroom. You need to break that door down and show them the exit.
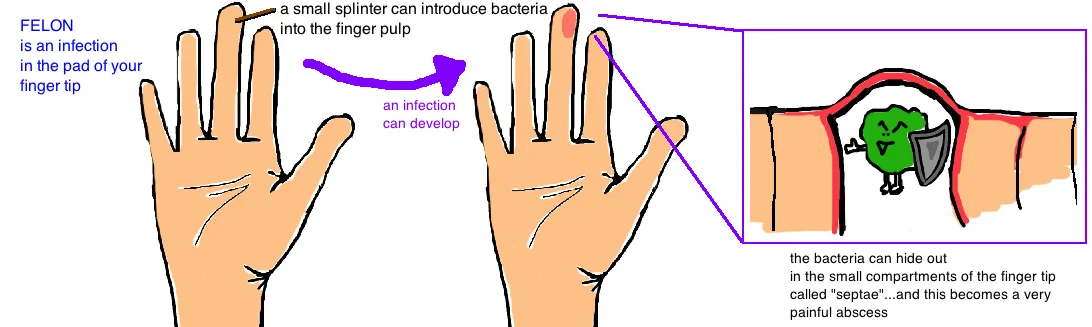
Felon
Another type of abscess, called a "Felon", occurs on the finger pad (opposite side of the finger as the nail infection).
The pulp of your finger pad is made up of lots of septations (small compartments made of very strong tissue) that forms strong connections between the skin and the underlying soft tissue to resist shear stress. This is what allows us to hold, grab, touch many things without this skin getting worn down and developing blisters at the fingertips. The problem is that bacteria can be introduced into these small compartments by a minor cut (like a splinter) and then collect within the small compartments. The infection will quickly cause inflammation, which leads to swelling, which leads to an elevated pressure within these small compartments. As the pressure rises above our blood pressure (the pressure our heart creates to pump blood), fresh blood carrying oxygen and nutrients cannot enter these small compartments and so the tissue dies. Unhealthy tissue in an area of infection is like a petri dish (bacteria love it) and this allows the abscess to get bigger. And bigger.
Even though these infections start small (remember all it takes is a paper cut or splinter), they can become extremely painful and need to be lanced. The lancing procedure should be performed by a doctor because the incision must be made along the outside of the finger (avoiding the finger's artery and nerve) and extend into the middle of the pulp to release the abscess. Incisions are made on the "pinky" side of the finger so that the thumb can still oppose these fingers without rubbing on the incision. Also if the incision doesn’t properly release all of the affected small compartments, the Felon has not been treated, and will continue to get worse. If not treated at all, osteomyelitis (an infection of the bone) can occur, which often requires weeks of IV antibiotics for treatment. Once properly incised and drained, the finger should heal in 3-4 weeks.
Bite Infections
Infections that form abscesses can also be caused from bites, either by animals or humans. Both humans and animals carry a lot of bacteria in their mouth, and so a skin laceration caused by a bite has a high risk for becoming infected.
A finger laceration caused by a human its usually the result of someone punching another and hitting their tooth (aka a fight bite). This can lead to pretty severe infections usually caused by multiple types of bacteria (although the most common infection is caused by eikenella bacteria). Treatment requires antibiotics (unasyn or augmentin) and usually an incision and drainage of any abscess that has formed.
If bitten by an animal, the main bacteria of concern is pasteurella, which requires similar antibiotics for treatment. House cats cause particularly bad abscesses that form rapidly after a bite (within 24 hours) and can cause significant redness and swelling. A cat bite is particularly bad because their teeth are very pointy and leave very small puncture wounds that allow the skin to close right back up after the bite. This traps all the bacteria within the hand and encourages the formation of an abscess. The best treatment, maybe contrary to what you would think, is to make the puncture wound a little bigger so the pus and bacteria can drain out of the body.
Flexor Tenosynovitis
The final type of bacterial infection that will be discussed, which is not very common, but requires urgent surgical treatment is a condition called flexor tenosynovitis.
The flexor tendon sheath surrounds our finger tendons and allows the tendons to glide smoothly as they move our fingers. A flexor tenosynovitis is an infection of this sheath that leads to inflammation and permanent scarring. Scarring prevents the smooth gliding motion of our finger tendons and therefore limits the mobility of our fingers.
The classic signs of flexor tenosynotivits were described by Dr. Kanavel: 1) a finger in semi-flexed position, 2) extreme pain when trying to straighten out the finger, 3) fusiform swelling (the finger looks like a big sausage); and 4) pain when you tap along the flexor tendon more proximally to the finger.
If this condition is suspected, a doctor will start IV antibiotics immediately. If the finger doesn’t show signs of improvement within 12 hours, then surgery is needed to flush the bacteria out of the sheath. The surgical incision is not immediately closed, but rather left open to allow everything to continue to drain for the next 2-3 days. If the finger shows improvement, the skin is closed with sutures. If there is no improvement, repeat surgery is required to wash out any remaining bacteria. The patient will continue IV antibiotics for 7-10 days and will then take antibiotics by mouth for a total of 4 weeks (its a lot of antibiotics but its important that every last bacteria gets eliminated). Patients will often complain of some post-infection stiffness, even if treated quickly. The goal is to preserve as much hand function as possible.
Fungal Nail Infection
Another common infection that is seen by hand surgeons is a fungal infection of the nail plate. The infection is actually under the nail, in the subungual region. These are called onychomycosis, or chronic fungal infection.
These infections treated initially with local antibiotic ointments. The affected nail may be treated every day for up to 6 months with this topical ointment. If this treatment fails to eliminate the infection, an anti-fungal medications can be taken by mouth (like terbinafine or itraconazole) which are taken for 2 months. These medications enter your blood stream and treat your entire body (sometimes they can injury your liver, so doctors much check your liver to make sure its healthy before giving the medication). If this medication still doesn’t cure the infection, which is the case in about 25% of such infections, then surgery is needed. Surgery consists of removing the whole finger nail, applying mycolognystatin (ointment) directly to the underlying nail bed, and allowing a new nail (clean and fungus free) to regrow. This treatment is usually effective, but it can be painful and there is always a risk the nail regrows looking abnormal. Therefore its the last choice in treatment.
Reference
1) Tosti R, Llyas AM et al. Empiric antibiotics for acute infections of the hand. J Hand Surg 2010; 125-128. full article.
2) McDonald LS et al. Hand infections. J Hand Surg 2011; 36A; 1403-1412. full article.
3) Tannan SC, Deal DN. Diagnosis and management of the acute felon: evidence-based review. J Hand Surg 2012; 37: 2603-4. full article. review.
4) Canales FL. The treatment of felons and paronychias. Hand Clin 1989; 5: 515-523. full article.
5) Hitchcock TF, Amadio PC. Fungal infections. Hand Clin 1989; 5: 599-611. full article.
6) Zubowicz VN, Gravier M. Management of early human bites of the hand: a prospective randomized study. PRS 1991; 88: 111-114. full article.
7) Abrams RA, Botte MJ. Hand infections: treatment recommendations for specific types. JAAOS 1996; 4: 219-230. full article.
8) Pang HN et al. Factors affecting the prognosis of pyogenic flexor tenosynovitis. JBJS 2007; 89A: 1742-1748. full article.
9) Jaffe AC. Animal bites. Ped Clin North Am 1983; 30: 405-413. full article.